Antidepressant Medications: Classes, Doses & Side Effects
Treatment resistant depression patients often come to Manlove Brain + Body Health believing they have tried “every antidepressant medication available”, though that is rarely the case.
Unfortunately, psychopharmacology has historically had only one approach to the treatment of depression since the 1950s based on the monoamine hypothesis, which posits that the underlying cause of depression is a depletion of serotonin, norepinephrine and/or dopamine neurotransmitters in the brain.
Therefore, antidepressant medications primarily increase the effects of these neurotransmitters by allowing them to remain longer in the neuronal synapse (the space between neurons), creating a stronger signal passing from one neuron to the next. Certain individuals, based on genetic makeup, may have lower levels of these neurotransmitters. Put simply, antidepressant medications enhance what your brain does naturally.
However, a genome study of 1.2 million people identified 178 gene variants linked to depression.
Despite the large number of genetic variations potentially contributing to depression and the limited approaches in treating it through enhancing neurotransmitters, antidepressant medications are still effective in approximately two-thirds of people who try them (though frequently with side effects) and 10% of the US population are currently taking antidepressant medications. The one-third of depression patients who do not find relief from these antidepressants are designated “treatment-resistant.”
All too often, treatment-resistant patients may, in fact, be very treatable with antidepressants. A patient’s treatment-resistance to antidepressant medication is often caused by one of three scenarios:
- The patient has tried multiple antidepressants, but all in the same class of antidepressant medication,
- The dosage may be insufficient to be effective, or
- The prescription does not take advantage of combined medications to create a synergistic effect.
Understandably, the “treatment resistant” patient is left feeling hopeless.
Because of the complexity of neuropsychopharmacology, it is important that you see a prescriber who is knowledgeable and experienced in prescribing specifically for mental health. While any physician (such as an Ob/Gyn, primary care provider, Oncologist, Cardiologist, etc.) can write a prescription for psychiatric medications, it is unrealistic to expect them to understand the nuanced differences between antidepressant medications, doses, side effects, and augmentation strategies. A psychiatrist, psychiatric nurse practitioner, or physician assistant trained in psychiatry will have the detailed knowledge and experience needed for treatment-resistant patients. When it seems like there is no hope, their expertise can make a life-changing difference.
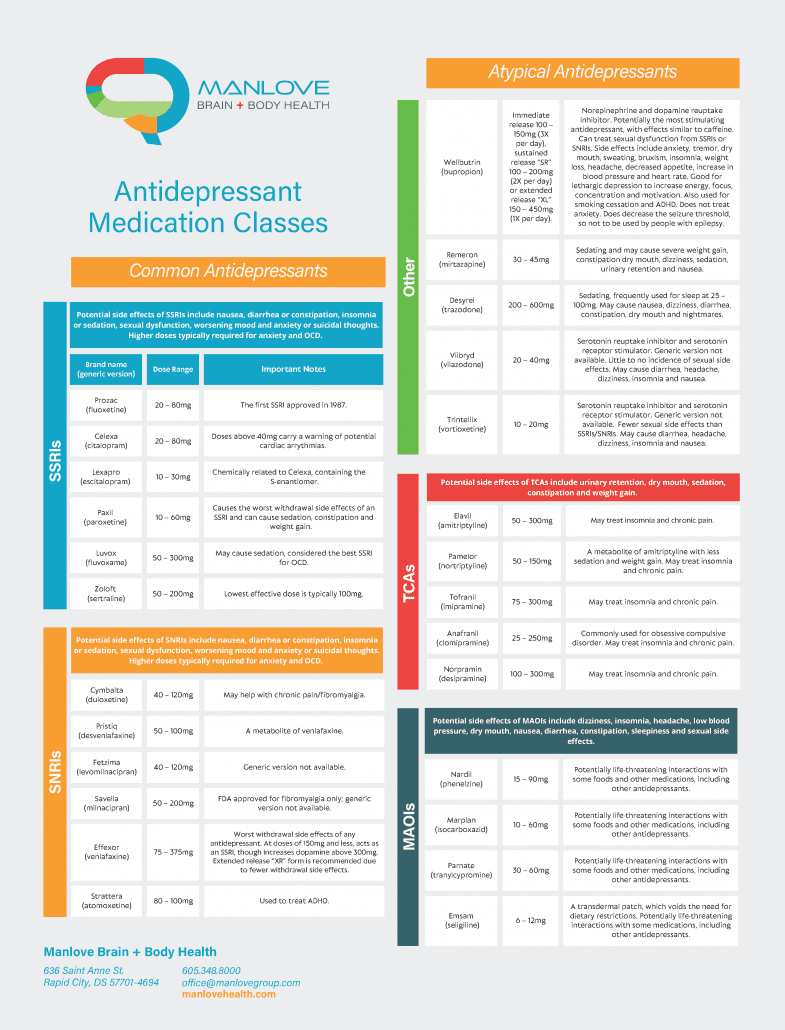
This outline below can also help provide some additional guidance.
Selective Serotonin Reuptake Inhibitors (SSRIs):
SSRIs are the most widely prescribed antidepressant medications. They are also used to treat anxiety, PTSD, OCD, and eating disorders. Anxiety treatment often requires higher doses than other disorders and OCD treatment may require doses above FDA recommended maximums.
SSRIs can be combined with medications from another antidepressant class for a synergistic effect, though not with others that also increase serotonin, or there is a risk of developing serotonin syndrome, a potentially life-threatening condition that involves autonomic instability (the inability of the body to regulate its homeostatic processes such as temperature).
Examples of antidepressant medication combinations include an SSRI plus another antidepressant, such as Wellbutrin (bupropion) or Remeron (mirtazapine), or an augmentation strategy, such as an antipsychotic/mood stabilizer, thyroid hormone or stimulant (Adderall, Ritalin, Vyvanse).
One consideration when choosing an antidepressant is that if a medication from one class didn’t work or caused side effects (such as an SSRI), you may wish to consider trying a medication from another class (such as an SNRI).
People also frequently find that the dose of an antidepressant medication may need to be increased either to achieve a greater benefit or because its effect lessens over time. The FDA recommended maximum dose provides a guideline where higher doses don’t seem to be more effective for most people and have a risk for potentially greater side effects.
Doses are typically lower for children and older adults. Common side effects of SSRIs include diarrhea, nausea and gas (because there is also serotonin in the intestinal tract), as well as sexual side effects.
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs):
SNRIs increase both serotonin and norepinephrine, essentially giving you “two for the price of one.” These medications are used for similar indications as SSRIs, and several can also treat chronic pain, fibromyalgia and ADHD. SNRIs and SSRIs should not be combined due to a risk of serotonin syndrome. However, other antidepressant medications with a different mechanism of action can be combined with SNRIs, such as Wellbutrin (bupropion), Remeron (mirtazapine), or mood stabilizer/antipsychotics, stimulant medications (Adderall, Ritalin), thyroid hormone, etc.
There is no evidence that SNRIs work better than SSRIs, though some people may be more likely to respond to SNRIs depending on their genetic makeup. This can be determined through genetic testing available through a number of different companies, such as Genesight or Genomind. Some insurers cover this service. If not, it can cost $350 to $400.
Atypical Antidepressant Medications
Monoamine oxidase inhibitors (MAOIs):
MAOIs are potentially considered the most effective antidepressants, as they increase three neurotransmitters simultaneously (dopamine, serotonin and norepinephrine). However, their use is limited by potentially life-threatening interactions with other medications and some foods. Common side effects are dizziness, insomnia, tachycardia, dry mouth, and low blood pressure.
While taking an MAOI, the enzyme that typically regulates tyramine levels is restricted. When this happens, your tyramine levels can get dangerously high, and cause blood vessel narrowing and blood pressure to skyrocket. Protein-rich foods typically contain high amounts of tyramine and should be avoided while taking MAOIs. It is also recommended to avoid eating leftovers, as tyramine levels in food increase during the decay process. Though expensive, the EMSAM patch is an MAOI that avoids potential food interactions and is replaced every 24 hours.
Tricyclic antidepressants (TCAs)
TCAs impact both serotonin and norepinephrine and have been around since the 1950s. They can be as effective as newer medications but typically have more side effects, including dry mouth, sedation, constipation, blurry vision, urinary retention, tachycardia, sexual dysfunction and weight gain. These medications are cardiotoxic in overdose. They are frequently prescribed at low doses to aid with sleep, headaches, and chronic pain, including fibromyalgia.
In addition to antidepressant medications included in the reference sheet above, there are a number of other medications that can also be added as augmentation strategies, including mood stabilizers, stimulants, hormones, anxiolytics and nutritional supplements, as well as transcranial magnetic stimulation (TMS), vagal nerve stimulation (VNS), ketamine, esketamine and numerous therapy treatment approaches.
When it feels like nothing will solve your depression, anxiety, or PTSD, don’t give up. It is most likely that your depression cannot be solved with common antidepressant medications, but there are many other options available. Give us a call at 605-348-8000 or find a psychiatrist in your area who can provide you with a personalized depression management plan.

Stephen Manlove, MD is one of the most entrepreneurial psychiatrists in the upper Midwest. Dr. Manlove graduated from the University of Minnesota Medical School and completed residencies in Psychiatry and Internal Medicine through the University of Virginia Medical School. He holds multiple board certifications in psychiatry/neurology, internal medicine and forensic psychiatry. This deep understanding of medicine gives him a unique ability to practice truly holistic psychiatry—fusing lifestyle changes and brain health best practices with genetic testing and a detailed laboratory workup to develop a personalized plan for each patient. As an early adopter of transcranial magnetic stimulation (TMS) and ketamine/Spravato, he and the Manlove Brain + Body team have helped thousands of patients suffering from treatment resistant depression, anxiety and PTSD.